Brief introductions to ongoing Nordic research projects on childhood cancer predisposition and genetic susceptibility testing.
Skip to:
ChiCaP, PeCCaPS, PROTECT-CARE, STAGING
CPS = Cancer Predisposition Syndrome
ChiCaP = Childhood Cancer Predisposition
WGS = Whole Genome Sequencing
ChiCaP from Sweden
The Childhood Cancer Predisposition Project

Almost every day one child is diagnosed with cancer in Sweden. Thanks to modern sequencing methods, knowledge about genetic cancer predisposition has increased in recent years. Today we know that at least 10% of children with cancer have an underlying genetic condition that increases their risk of developing cancer. ChiCaP is more common in children with rare tumors, adult cancer types, multiple primary tumors, excessive toxicity to treatment, congenital anomalies, overgrowth, immune deficiencies, hematological or skin disorders and in children with consanguineous parents or a family history of cancer at an early age among close relatives.
It is of great importance to recognize ChiCaP, since it can lead to adjusted cancer treatments, surveillance programs, and may allow genetic counselling, and testing of family members. However, most ChiCaP diagnoses have until today escaped detection since the underlying ChiCaP diagnoses are heterogenous. Diagnosis of ChiCaP requires broad genetic testing, careful phenotyping, and expertise in interpretation of genotype/phenotype findings.
A unique national collaboration “GMS Childhood cancer” has been established between Genomic Medicine Sweden (GMS), the Swedish healthcare system, the Childhood Tumor Bank and the Nordic Childhood Leukemia Biobank to offer whole genome sequencing (WGS) in tumor and germline to all children with cancer.
ChiCaP Genetic Study
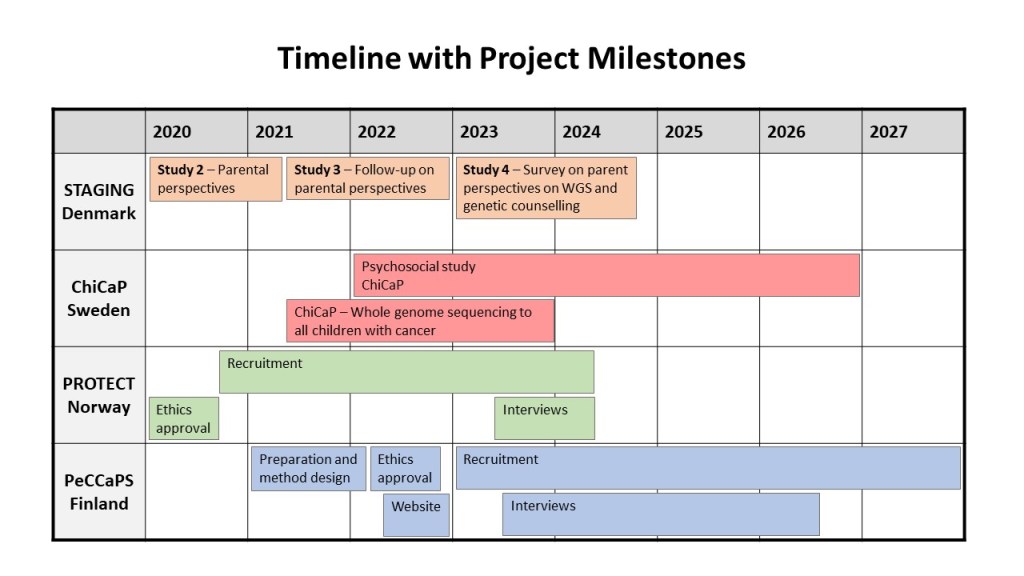
The Childhood Cancer Predisposition (ChiCaP) project, that is part of the “GMS Childhood cancer”, aims to better understand the genetic predisposition in childhood cancer and to introduce germline testing in clinical practice. The national project is led by Ann Nordgren and supported by the Swedish Childhood Cancer Fund. The project has been running since Spring 2021 and so far, more than 300 children have been included in the study. All six pediatric oncology centers in Sweden are part of the study and whole genome sequencing (WGS) is centralized to three regions. Both the tumor and germline genomes are investigated simultaneously and the ChiCaP project focuses on investigating the germline genome.
A specific questionnaire “ChiCaP criteria” has been developed to systematically collect family history, cancer type and history, as well as other phenotypic findings to assess the risk of cancer predisposition in the child and to guide the genetic analysis. After sequencing, germline WGS data is both used for the somatic analysis and for germline testing. In the ChiCaP research project we are testing two tracks, a “clinical track” that we plan to introduce in the clinic in the end of the project and a “research track”. Bianca Tesi is coordinating the “clinical track” and Fulya Taylan the “research track”.
Clinical track
In the “clinical track”, that is already performed in close collaboration with the clinic, two different in silico gene panels are used based on the information provided in the “ChiCaP criteria” questionnaire. All children are tested with the “ChiCaP Actionable” gene panel that includes 56 well established ChiCaP genes with clear treatment recommendation and children with positive ChiCaP criteria are investigated with a broader gene panel “ChiCaP Clinical”, consisting of 189 genes that also include the ChiCaP actionable genes. All genetic findings that are discovered in the “clinical track, are directly reported back to the pediatric oncologists in the clinic and acted upon.
Research track
In the “research track”, a more extensive gene panel (n=862) is used to discover new genes and pathways associated with cancer predisposition. The overarching goal is to analyze WGS results from over 400 pediatric patients with solid tumors in a rare variants association study (RVAS). Furthermore, cases with strong family history of cancer and/or other phenotypic findings, such as intellectual disability and congenital malformations, will be further investigated by performing WGS trios where the child’s genome will be compared to the parents’ genome.
Overall, the ambition of the project is to better understand the underlying genetic etiology of different cancers in children, provide accurate and timely diagnoses, classify the risk groups, identify at-risk members, tailor the treatment, and provide surveillance programs and genetic counselling, with the ultimate goal to save more lives.
ChiCaP Psychosocial Study
Impact of testing for ChiCaP at cancer diagnosis
Even though it is of great clinical importance to diagnose ChiCaP, genetic testing for ChiCaP in children with cancer may cause additional anxiety and stress for the parents in an already extremely stressful situation. The overall aim of the Psychosocial ChiCaP study is to explore parents´ experiences before, during and after genetic testing for ChiCaP. Similar questionnaire are distributed to families in Norway and Australia and the Nordic ChiCaP network is currently harmonizing the questions that will be used in the interviews . We want to increase our understanding of how parents perceive genetic information andif they are well informed before germline genetic testing for ChiCaP in their child. We also want to investigate how parents experience the diagnostic process until return of test results and if there is need for more information and support. We want to understand the psychological impacts for parents of children with cancer who have been diagnosed with ChiCaP and how knowledge about ChiCaP affect the families.
Parents to children with cancer, undergoing WGS within the GMS Childhood cancer predisposition study are invited to participate in the study. After signed informed consents they are asked to fill in two questionnaires; one prior to genetic testing and another after receiving test results. We will also perform deep interviewes of parents to children where the genetic analyses have revealed cancer predisposition in the child in order to investigate their experiences and perceptions of testing and how the ChiCaP diagnosis has affected their lives. Our goal is to develop a robust and ethically sound method, based on parents´ views, to perform WGS to identify ChiCaP in a clinical setting. This study can potentially lead to changed and improved routines within clinical diagnostic activities.
Links to funding bodies are below.
PeCCaPS from Finland
Personal Crisis & Cancer Predisposition Syndromes
Multidisciplinary nationwide prospective clinical study
Research objectives and areas of interest:
- National model for genetic counseling
- Psychosocial outcomes of genetic testing
- actors responsible for different responses
- Individual needs of parents and families
- Testing Finnish MICRA for impacts on parents
This prospective clinical study aims to investigate how parents experience and perceive genetic testing for cancer susceptibility that is performed on their children. The study focuses on information needs, longitudinal psychosocial effects, sense-making and integration, standardisation of testing, and the advancement of genetic counselling. This is a nationwide translational project, involving pediatric haemato-oncologists, geneticists, psychologists, and bioethicists.
Links to funding bodies are below.
To contact the project team, please email us at peccaps@utu.fi
PROTECT-CARE from Norway
Precision Oncology Targeting Early life Cancer diagnosis and Therapy – Germline project (webpage)
Research objectives and areas of interest:
- Frequency, actionability, and clinical impact of CPS
- Gene discoveries from unusual phenotypes
- Patient and familial perspectives and concerns
- Informing ethical & patient-centered care
Target groups:
Parents & Children
Our research through PROTECT will address ethical and psychological aspects of germline testing in children with cancer, as well as increase knowledge about the genomic variants and clinical applicability of germline and tumor genomics in our Norwegian childhood cancer population. The PROTECT collaboration will then apply this knowledge to directly impact health service organization and quality, through establishing an ethically sound genetic predisposition pipeline for childhood cancer patients, and guidelines for different pediatric tumor testing modalities and interpretations in separate cancer settings.
The PROTECT germline study completed inclusion in February 2022, and we are at the moment analyzing data and preparing articles for release. We plan to expand the part of the PROTECT project addressing ethical and psychological aspects with the Psycho-Social and Clinical Communication aspects of childhood cancer predisposition testing (PROTECT-PSCC). Here we will seek to generate called for knowledge about the psychosocial impact of CPS testing, the information and support needs of the involved families and health care personnel, and to develop new tools for communication and implementing them in clinical practice to better meet the needs of health care personnel and families.
STAGING from Denmark
Sequencing Tumor And Germline DNA Implications and National Guidelines (with psychosocial sub-studies)
Research objectives and areas of interest:
- Parental experiences with the recruitment
- Practitioner perspectives on adopting WGS
- Families with clinically relevant findings
- Survey about genetic counseling and WGS
Target groups:
Parents & Practitioners
STAGING project aims to implement WGS of all newly diagnosed paediatric cancer patients in Denmark. The project maps the frequency of cancer predisposition syndromes in a consecutive national cohort of children with cancer. This knowledge is used for treatment adaptation, implementing relevant surveillance measures, and family planning. STAGING is a multidisciplinary project that combines clinical genetics, anthropology, paediatric oncology, and bioinformatics. Sub-study on parental perspectives was designed to document parental accounts of pragmatic, social, and ethical dilemmas related to research participation involving genetic counselling and WGS of childhood cancer patients. Another sub-study was designed to investigate how practitioners perceived and reacted to the introduction of WGS. This study surveyed pediatric oncologists, clinical geneticists, and nurses.